Use of Standard Field Surgical Telescopes During Penile Implant Surgery for ED
Background:
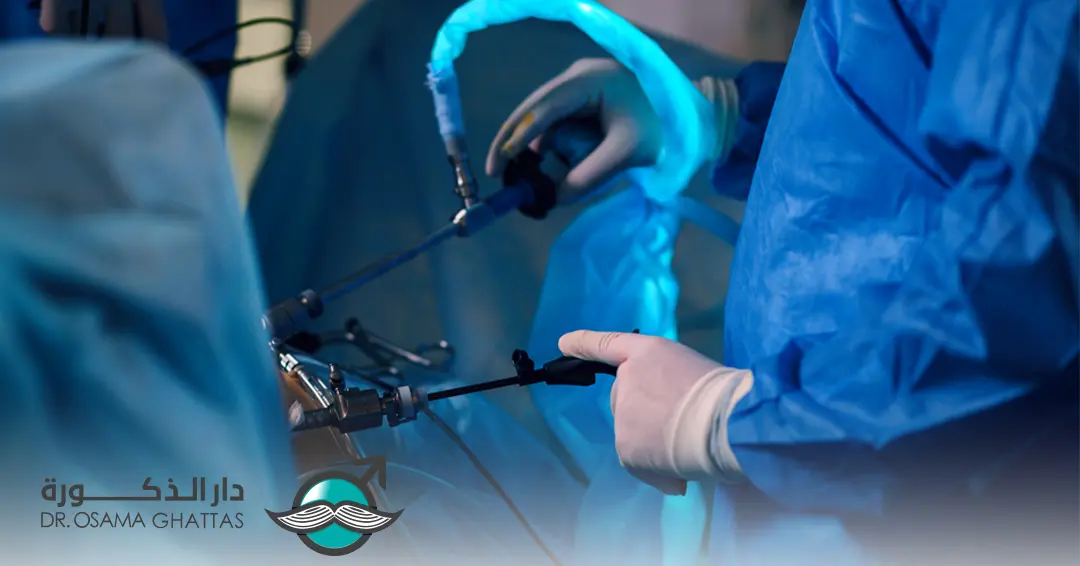
- Penile prosthesis implantation is a technically nuanced urologic procedure, typically performed through an open approach with direct visualization and tactile guidance. The surgeon relies on corporal dilators, sizers, and retractors to access the corpora cavernosa and prepare the space for implant insertion. While some have proposed the use of endoscopic tools (rigid or flexible telescopes) to enhance visualization, this approach has not become part of routine practice.
Why Telescope Use Is Not Optimal in Routine Settings?
Despite the potential benefits, standard field surgical telescopes present several practical and clinical limitations that make them suboptimal for routine use in most penile prosthesis surgeries:
- Disruption of Established Surgical Workflow
– Penile implant surgery is typically efficient, with a well-established workflow that emphasizes direct exposure and tactile feedback. Introducing a telescope requires a shift in technique. This disrupts the surgeon’s rhythm and slows down the procedure — without significant benefit in straightforward cases.
– Anatomically, the primary neurovascular bundle supplying the penis runs along its dorsal surface. In contrast, the surgical incision for penile prosthesis implantation is made on the ventral aspect, well away from this bundle. The ventral surface contains no major arteries or nerves at risk of injury during this procedure. The only critical structure in this area is the urethra, which is easily visible to the naked eye during surgery. Therefore, there is no justification for using surgical magnification in standard penile implant procedures, unlike surgeries involving penile curvature correction or reconstruction, where dissection of the dorsal neurovascular bundle is often required.
– The notion that surgical magnification is necessary during prosthesis implantation to preserve the cavernous artery and, by extension, the erectile tissue, is both scientifically inaccurate and practically unfeasible for several reasons:
Complex Vascular Architecture:
The cavernous artery is not a single, isolated vessel—it gives rise to hundreds or thousands of helicine arteries along the corpus cavernosum. These minute, fragile branches are embedded within erectile tissue. Any mechanical disruption, such as surgical dilation, inevitably damages them. Preserving a single segment of the main artery does not prevent overall vascular compromise if these branches are torn.
Role of Venous Drainage:
Healthy tissue perfusion depends not only on arterial inflow but also on venous outflow. The emissary veins responsible for drainage from the corpus cavernosum are numerous and microscopic, arranged circumferentially along the cavernosal wall. When the tunica albuginea is incised and dilators are used, these veins are invariably damaged, disrupting the entire vascular integrity of the corpus cavernosum. Thus, preserving the artery alone is insufficient and ineffective.
Limitations of Surgical Access:
The incision made into the corpus cavernosum during implantation is typically 1–2 cm long, whereas the corpus cavernosum itself may extend over 20 cm. Even if microscopic preservation of the artery were theoretically possible at the incision site (which is unlikely), it would be impossible to do so along the entire length of the penis, especially during blind dilation of proximal and distal segments, including those in the pelvic region.
– The concept of preserving cavernous tissue or arteries during penile prosthesis surgery is a theoretical construct with no practical feasibility. Claims suggesting that surgical magnification can achieve this are not grounded in anatomical reality or surgical practice. Using such arguments to justify magnification appears more as a marketing tactic than a clinical necessity. - Minimal Added Value in Uncomplicated Cases
– In primary penile prosthesis surgeries involving non-fibrotic, compliant corporal tissue, the added visualization offers limited clinical advantage. Open exposure already provides adequate visibility, and the surgeon’s tactile sense remains more reliable than an image-based assessment when dilating corpora or inserting cylinders. Thus, the use of a telescope in these settings adds complexity without enhancing safety or outcomes.
Conclusion:
- Current literature does not provide strong evidence to support the routine use of it during penile implant surgery.
- While the selective use of a telescope may be beneficial in complex scenarios—such as revision surgeries, severe corporal fibrosis, Peyronie’s disease, or prior priapism—its routine application in all penile implant procedures is neither supported by evidence nor justified by clinical benefit. In these routine cases, the drawbacks—added time, cost, risk, and workflow disruption—outweigh the theoretical advantages. Thus, standard field surgical telescopes should be viewed as an adjunct for specific, high-difficulty situations rather than a default tool in prosthetic urology.
References:
- Henry, G. D., Mahle, P., Caso, J., Eisenhart, E., Carrion, R., & Kramer, A. (2015). Surgical techniques in penoscrotal implantation of an inflatable penile prosthesis: a guide to increasing patient satisfaction and surgeon ease. Sexual medicine reviews, 3(1), 36-47.
- Köhler, Tobias S., Ricardo Munarriz, Justin Parker, Carlo Bettocchi, Georgios Hatzichristodoulou, Francisco E. Martins, Ignacio Moncada et al. “Penile prosthesis for erectile dysfunction: recommendations from the 5th International Consultation on Sexual Medicine.” Sexual Medicine Reviews13, no. 2 (2025): 144-171.
- Chang, Chrystal, David W. Barham, Zafardjan Dalimov, Daniel Swerdloff, Hossein Sadeghi‐Nejad, Robert Andrianne, Maxime Sempels et al. “New findings regarding predictors of Poor Corporal Integrity in Penile Implant Recipients: A Multicenter International Invesigation.” BJU international 135, no. 3 (2025): 528-534.
- Tomada, Nuno, Elena Martínez-Holguín, and Enrique Lledo Garcia. “Step-by-step implant in severe fibrosis.” In Penile Prosthetic Surgery, pp. 259-274. Academic Press, 2025.
- Bettocchi, Carlo, Anna Ricapito, Matteo Rubino, Michele Di Nauta, Gian Maria Busetto, Luigi Cormio, and Giuseppe Carrieri. “Ongoing research future of the penile implant.” In Penile Prosthetic Surgery, pp. 337-352. Academic Press, 2025.
- Falcone, Marco, and Lorenzo Cirigliano. “Semirigid penile prosthesis implantation.” In Penile Prosthetic Surgery, pp. 105-113. Academic Press, 2025.
- Li, Yingxi, Dawei Gao, Jingyi Zhang, Meijing Wang, Xiucheng Lan, Xujun Yu, and Degui Chang. “Penile prosthesis implantation: a bibliometric-based visualization study.” International Journal of Impotence Research 37, no. 1 (2025): 4-13.